Cervical cancer (CC) is the fourth most common cancer in women worldwide and it is the 2nd most common cancer in Bangladesh. The incidence of CC was 8068 and 5214 women died from CC in the year 2018. CC constitutes about 12% of female cancer in this country.
We all know prevention is better than cure. The Government of Bangladesh (GOB) adopted visual inspection of the cervix with acetic acid (VIA) method for cervical cancer screening for the women of 30 years and above every 5 years. The GOB has extended the program to 431 centers at districts and upazilas. VIA +ve women are attending at the colposcopy clinics of BSMMU, and different MCHs for colposcopic evaluation and management. In Bangladesh, colposcopy became an important part of the prevention program both for diagnosis and guiding the treatment and with increasing awareness, gradually increasing number of women will attend private facilities for screening and evaluation.
Basic Colposcopy training held at least twice a year. Our society arranged training of 11 batches and so far 90 doctors received training. Advanced colposcopy training was given to doctors. After completion of the Basic training, trainees are given a provisional certificate. Once they fill up the Log book, they should undergone final assessment for certification.
It is worth to mention that BDSCCP is encouraging colposcopy training for junior doctors and doctors practicing for less than 5 years at a very low cost of a duration of 6 days. Society encourages the members for attending colposcopy related scientific programs as well.
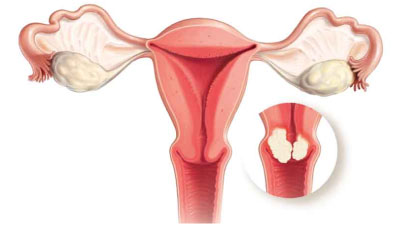
Cervical cancer
- It is the leading cause of deaths of women in developing countries.
- Eighteen percent of cancer infected women die due to cervical cancer in Bangladesh.
- Every year more than 11,000 women die due to cervical cancer.
- It means in Bangladesh everyday average 28 women die in cervical cancer.
Barrier for early Diagnosis
- Cervical cancer is symptoms less in early precancerous or micro invasive stage.
- So women in Bangladesh don’t seek any advise without symptoms.
- They seek health care in advanced stage of cervical cancer when they have symptoms and at that time the outcome is not so effective.
- They seek health care in advanced stage of cervical cancer when they have symptoms and at that time the outcome is not so effective.
- In Bangladesh Cultural factor is also a very big factor that acts as a barrier for early diagnosis.
- The most important factors affecting the women’s ability to make decision since husbands have to be consulted or informed before seeking any treatment .
- For that reason they don’t go for availing screening facility or early treatment .
Barrier for early treatment
- Lack of awareness of the benefits of the screening test considering oneself not at risk
- Fear of getting diagnosed as cancer and embarrassment
- In south Asian countries like Bangladesh, India, Nepal, women refused to be screened, out of fear of the potential social stigma.
Pretreatment Staging
- It defines the clinical staging system for cervical carcinoma based on clinical assessments.
- It includes physical examinations at out patients departments with reasonable accuracy.
- Examinations under anesthesia may be required for some of the obese patients with early stage cancer or such patients where examinations at out patients department is not possible due to some disability.
- Each and every patients should have a thorough pelvic examination that includes inspection, palpation to note the position & size of the cervical growth, extension to the vagina & parametrial tissue.
- Vesical involvement should be suspected if there is extensive involvement of anterior vaginal wall by a large growth with induration of the bladder base.
- Rectal examination is very valuable to diagnose the nature and extent of parametrial involvement and infiltration of the disease to the rectal mucosa.
- Rectovaginal examination, is a relatively simple type of pelvic examination, performed by examining the vaginal area and the rectal area at the same time. This also allows to better determination of the nature and extent of parametrial involvement and infiltration of the disease to the rectal mucosa.
- Colposcopy should be done where there is obvious indication like VIA (Visual Inspection of cervix with acetic acid) &Paps smear positive, postcoital bleeding, suspicious cervix ,where cervix bleeds on touch.
- Colposcopy is also useful to note the extent of the tumor in the vagina and the presence of vaginal intraepithelial Neoplasia (VAIN) .
- Endocervical curettage and /or hysteroscopy should be done where there is abnormal uterine bleeding.
- Study shows there is a is good agreement between grade of dysplasia on preoperative ECC and on subsequent conization specimen.
- Colposcopic examination is not a good predictor for the pathology in the endocervical canal
- Routine ECC should be a part of the preoperative assessment of an abnormal Papanicolaou smear and abnormal uterine bleeding.
- The current official staging system for cervical cancer is based on the International Federation of Gynecology and Obstetrics (FIGO) classification .
- Different studies shows errors in clinical FIGO staging.
- Under staging of Ib–IIIb cancer varying from 20%–40%.
- Over staging of FIGO IIIb cancer in up to 64%.
- Cystoscopy and proct-sigmoidoscopy should be performed if there are clinical and /or radiological suspicions of bladder and rectal involvement respectively.
- Bladder and rectal mucosa involvement has to be proved by histology for the disease to be considered stage IV disease.
- Only bullous edema of the bladder on cystoscopy does not confirm malignant infiltration of bladder mucosa.
- Additional information may be obtained from Computed tomography (CT),magnetic resonance imaging (MRI)and positron emission tomography (PET)scans.
Radiological Staging
- Radiological assessment of patients with visible cervical carcinoma is an essential part of the strategy in determining the most appropriate management of patients.
- Both at primary presentation and with relapsed disease or complications of treatment.
- Pelvic and abdominal sonography has replaced the routine intravenous urography to exclude hydroureter and hydronephrosis.
- Sonography provides additional information like size of growth possible invasion of bladder and rectum, metastasis to liver etc.
- There is consistent evidence that MRI is more accurate than CT for radiological staging of cervical carcinoma (accuracies 40–97%)
- Both modalities are more accurate than clinical staging
- Assessment of bladder and rectal invasion is consistently more accurate with CT and MRI than clinical staging.
- With the specificity of MRI considerably greater than CT.
- Primary tumor volume is best assessed by MRI rather than CT.
- Tumor diameter less than 5-10 mm cannot be reliably imaged by either modality.
- Post-biopsy changes may also adversely affect tumor measurement, particularly in small tumors.
- Appearances following a loop excision biopsy or cone biopsy cause difficulty in assessing the size and extent of the primary tumor.
- Which may have important staging and prognostic consequences.
- There is some evidence that PET scans may also measure tumor volume but false negative uptake also occurs following excision biopsy.
- Vaginal invasion is best assessed by MRI, with accuracies ranging from 78-94%.
- Over staging errors are reported in association with bulky primary tumors distending the fornices.
- CT staging accuracies are not available.
- Involvement of parametrium indicates inoperable FIGO IIB disease.
- Studies report shows variable accuracy for parametrial staging by MRI and CT.
- MRI is generally superior to CT, with staging accuracy of 75-90%.
- Full thickness disruption of the ring of cervical stroma by tumor on MRI corresponds to FIGO stage IIB disease.
- Confirmation of an intact ring of cervical stroma, on adequate MRI assessment, confers potentially operable status.
- PET imaging alone cannot accurately determine early parametrial involvement.
- Several studies show 100% negative predictive values for CT and MRI in bladder, rectal and ureteric invasion.
- A normal appearance of bladder and rectum on MRI examination obviates the need for cystoscopy or sigmoidoscopy.
- Intravenous urography (IVU) has been superseded as a stand alone investigation, as CT, MRI or ultrasound are as accurate in determining ureteric obstruction secondary to parametrial invasion and give additional information.
- Barium enemas are not routinely indicated.
- pelvic or Para-aortic lymph nodes Although not a part of the FIGO staging criteria, the involvement of pelvic or Para-aortic lymph nodes in most histological types of cervical cancer, is the greatest single predictor of long term survival.
- Cannot be assessed by clinical examination alone.
- Imaging plays an essential role in pretreatment evaluation of women with invasive cervical cancer.
- It is used to assess tumor size and location; to detect involvement of the parametrium, pelvic sidewall, and adjacent organs; and to search for lymph node metastases.
- MRI provides the best visualization of the primary tumor, estimation of tumor size and volume, and extent of soft-tissue disease in the central pelvis.
- FDG-PET is the best modality in assessing nodal, extra pelvic, and bone metastasis and is also helpful in predicting patient outcome
Pretreatment evaluation
- Pathology reports of cervical tumors should include the following histological feature:
- Tumor type
- tumor size
- Extent of tumor (e.g. involvement of the vaginal wall or parametrium)
- Depth of invasion pattern of invasion (infiltrative or cohesive invasive front)
- Lymphovascular space invasion (LVSI)
- Depth of invasion pattern of invasion (infiltrative or cohesive invasive front)
- Lymphovascular space invasion (LVSI)
- Status of resection margins (presence of tumor and distance from margin)
- Status of lymph nodes (including site and number of nodes involved)
- Presence of pre-invasive disease.
- When assessing stromal involvement:
- All biopsy material should be taken into account
- It is important to be aware that a small tumor may be entirely removed by biopsy.
- Pathological assessment should be quality assured and standardized, with readily accessible specialist review available if required, following discussion by the multidisciplinary team.
SENTINEL node surgery
- There is evidence from a number of small case studies that it is feasible to identify sentinel lymph nodes during cervical cancer surgery.
- The evidence that the status of these nodes accurately predicts the status of the remaining pelvic lymph nodes is conflicting.
- At present there is no evidence to support the use of sentinel node surgery
Pelvic lymhadenectomy
- No evidence was identified to address the adequacy of pelvic lymphadenectomy specifically in cervical cancer.
- Evidence from many studies indicates that there is considerable variation in the number of lymph nodes obtained from this procedure.
- There is no evidence relating the number of lymph nodes retrieved to long term outcome.
- Many of the studies lack information about how the tissue is handled by the pathologist.
- Lack of good quality evidence illustrates the need for standardization of pathological assessment.